For hospital leaders tasked with managing unexpected surges in patient demand, the ability to anticipate and adapt to rapidly changing circumstances has become more essential than ever. What if we could predict potential bottlenecks in patient flow in real time – and prevent them before they occur?
While the pandemic has put critical care capacity under the spotlight like never before, hospitals around the world have long faced challenges with bed and staffing shortages to meet demand for acute care. Emergency departments (EDs) in many countries struggle with overcrowding even under regular circumstances. Intensive care units (ICUs) may be operating at or near capacity. All too often, waits and delays are the result – causing frustration, anxiety, and potentially harmful outcomes in patients, while adding to the pressure for staff [1].
It can be tempting to think that the solution lies in adding more beds or more staff. But typically, the problem is not merely one of resources. It’s also about better managing the beds you have. The real challenge is often one of patient flow: anticipating and knowing when to transition a patient from one care setting to the next.
It’s a highly complex and dynamic orchestration challenge, with many moving parts. Which patient waiting in the ED should get the next ICU bed? Which patient in the ICU can I safely move to a step-down unit to free up a bed? And who is ready to be discharged for home monitoring?
Managing patient flow requires an enterprise-wide view across different parts of the hospital or hospital network. However, that’s often precisely what’s missing today. With clinical and operational data dispersed across disparate systems, care teams lack wider situational awareness beyond their unit or department. It’s this lack of readily available and actionable information that can hamper patient prioritization, slow down patient transitions, and lead to unforeseen bottlenecks in patient flow.
The COVID-19 crisis has exposed and exacerbated many of these challenges. But it has also given rise to smart ways of tackling them. Healthcare providers have embraced centralized care collaboration models, sharing data in real time to visualize untapped capacity and facilitate patient transfers. And they’re not just relying on that data to get an overview of what’s happening from moment to moment. They’re also using it to forecast and prepare for future demand. For example, hospitals have successfully used predictive models to estimate the number of beds, equipment and staff needed for COVID-19 patients in the ICU and other hospital wards [2,3].
As we begin to think beyond the pandemic, there’s a unique opportunity to embed these data-driven practices into the everyday management of patient flow – from hospital admission all the way to hospital discharge and, ultimately, monitoring in the home. Using the power of AI and predictive modelling, we can extract relevant patterns and insights in patient flow and patient care needs from vast amounts of real-time and historical hospital data. After initial validation, the resulting algorithms can be updated on a regular basis to take recent trends and circumstances into account, thereby further optimizing predictive value. This enables hospital leaders and patient flow coordinators to orchestrate care more effectively across settings and rapidly adapt to changing circumstances.
Here’s what that may look like for one patient’s journey.

Anticipating next steps across the patient journey
Imagine a 66-year-old patient, Rosa, who is rushed to the hospital with heart palpitations and shortness of breath. As she is en route in the ambulance, a notification is sent to Jennifer: a patient flow coordinator in a central command center who oversees current and predicted patient capacity in a network of eight hospitals.
Because Jennifer can instantly see which hospitals have beds available, she is able to direct Rosa to a hospital where she’ll rapidly get the care she needs. If capacity trends indicate that certain hospitals are about to be overrun with patients in the coming 24 hours, for example due to a public emergency, Jennifer can start facilitating patient transfers to lower-census hospitals, thereby balancing patient load across the network. Or she can work with local supervisors across the hospital network to activate surge plans, open overflow beds, and plan for additional staffing. All to prevent ED overcrowding and delays in diagnosis and treatment.
As soon as Rosa is triaged in the ED, Jennifer can help care teams prioritize further clinical evaluation based on, among others, a machine learning algorithm that combines patient vital signs and physiological data to predict risk of health deterioration. Jennifer also has the latest overview of bed availability across the hospital, allowing her to pre-allocate a bed for Rosa in the right care unit, in close alignment with the team on the floor. In addition, Jennifer can see how many ventilators will be needed by each critical care unit for up to the next 48 hours.
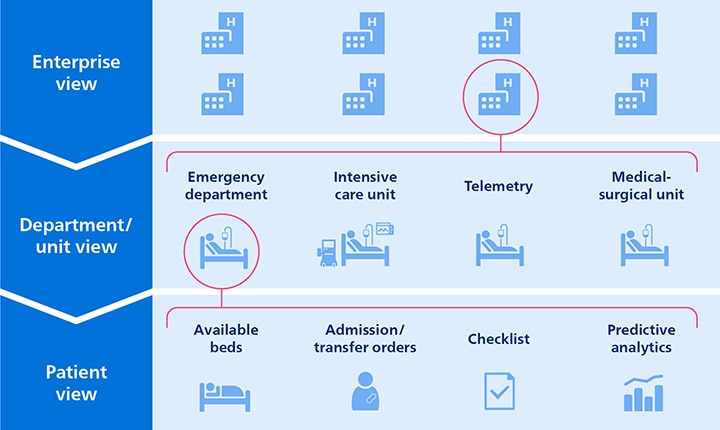
Once Rosa has received critical care in the ICU to help stabilize her condition, Jennifer can already start planning ahead to facilitate Rosa’s care journey. Smart algorithms support Jennifer in estimating when Rosa will be ready to be transferred to a lower-acuity care setting in the hospital for telemetry monitoring. Based on a transition review list that is updated dynamically, Jennifer can support physicians in prioritizing clinical evaluation of patients who may be ready for transfer. At the same time, she has an up-to-date overview of available telemetry monitoring. She can also see how many patients in the ED are waiting for an inpatient bed. This helps Jennifer identify potential bottlenecks early and manage patient flow accordingly.
Upon admission to a step-down unit where she is placed on telemetry monitoring, Rosa remains under the caring eye of clinical staff – with predictive algorithms again helping Jennifer orchestrate next steps proactively. Based on an analysis of physiologic deviations and alarm trends over the last 12 hours, Jennifer is able to evaluate when Rosa’s condition is stable enough for her to be considered for transfer to the medical-surgical unit.

We now come to the end of Rosa’s in-hospital care journey. As she’s being monitored in the medical-surgical unit – her last stop on the way to hospital discharge – Rosa’s discharge readiness score and readmission risk indicate that she is physiologically stable and well on her way to recovery. After the responsible physician has reviewed her condition, Rosa receives the reassuring message she has been waiting for. She is ready to go home.
Improving patient flow and reducing length of stay
With thousands of patients like Rosa flowing through a hospital network on any given day, it’s easy to see the benefits of having centralized clinical and operational insights to manage patient flow.
Rather than optimizing in silos, healthcare providers can start to orchestrate care across their entire enterprise. Add to that the power of predictive analytics, and it becomes possible to manage patient flow proactively from one care setting to the next. By accelerating patient progression through their care journey, healthcare providers can prevent congestion in certain areas of the hospital and overutilization of critical resources in others.
For a patient like Rosa, that means she doesn’t have to stay in the hospital any longer than necessary. This, in turn, gives other patients a better chance of getting access to the critical care they need. As a result, healthcare enterprises can serve more patients, thereby reducing backlogs in the wake of the pandemic. In addition, improved patient flow can also benefit their bottom line. For example, one US hospital estimated that they could save $3.9 million annually by eliminating ED overcrowding through accelerated transfers to inpatient settings [4].
Enabling networked decision-making across the hospital
For such enterprise-wide management of patient flow to work, more is needed than a central command center that monitors and orchestrates patient capacity and patient transitions. Together with all care teams involved, senior leadership will need to agree on relevant enterprise-wide KPIs that reflect real-time and anticipated patient flow across departments. In combination, those KPIs should give everyone a reliable forecast of impending bottlenecks as well as insight into appropriate interventions.
Information that helps to manage patient flow will also need to be available at the point of care, in an easy-to-use and actionable form that is visible to all team members – whether it’s through dashboards or well-timed alerts. Predictive insights should augment physicians in their decision-making and integrate naturally into their workflows, without adding to information overload.

Continuous adaptation is key here. Unlike some other industries such as manufacturing, where processes follow a fixed and predetermined sequence, healthcare is a human endeavor where unexpected events happen. For example, a patient like Rosa may not respond to her treatment plan as anticipated and need to be readmitted to the ICU for further intensive care. Predictive algorithms can help to pick up early signs of deterioration, but in-the-moment clinical judgment remains essential in assessing a patient’s condition and deciding what to do next.
That’s why central command centers in healthcare are not about top-down management. Rather, they should support collaboration among physicians and care administrators across the hospital or hospital network. The future of care will be all about predictive insights informing networked decision-making, with physicians and staff remaining in charge of clinical decisions, supported by a central hub that oversees the bigger operational picture to proactively manage patient flow.
Extending care coordination from the hospital to the home
In the future, centralized care coordination could be further extended into the home, using remote diagnostics and monitoring to keep a caring eye on Rosa as she resumes her daily life. As my colleague Roy Jakobs has outlined before, improving transitions between acute and post-acute care is one of healthcare’s biggest opportunities as it becomes increasingly distributed. Again, this is where predictive analytics in healthcare could make a difference.
Imagine that patient flow coordinator Jennifer gets an early warning signal that Rosa’s health is about to deteriorate again, based on a remote analysis of her vital signs and biometrics. This would allow Jennifer to proactively alert care teams to invite Rosa in for further clinical evaluation, preventing an avoidable emergency event later on. Ongoing health monitoring at home has already demonstrated its value in managing chronic diseases such as COPD, with one pilot study in the US showing an 80% reduction in acute 30-day COPD readmissions and $1.3 million in savings [5].
Ultimately, that is how healthcare systems of the future will manage patient flow more effectively and efficiently across the patient journey – relying on data-driven decisions to ensure that the right patient gets the right care in the right place at the right moment. Whether that’s in a hospital, the home, or a community setting. Based on a deeper understanding of patterns in patient demand and patient flow, healthcare leaders can also start creating long-term strategies for hospital capacity planning, making better informed decisions about the types of care settings and resources that are needed.
Uncertainty will remain as inherent to healthcare as it is to life. But by better forecasting what may happen next, healthcare systems will become more adaptive and resilient in the face of change and crisis. That’s a prediction I’m willing to make.
References
[1] Rutherford PA, Anderson A, Kotagal UR, Luther K, Provost LP, Ryckman FC, Taylor J. Achieving Hospital-wide Patient Flow (Second Edition). IHI White Paper. Boston, Massachusetts: Institute for Healthcare Improvement; 2020. http://www.ihi.org/resources/Pages/IHIWhitePapers/Achieving-Hospital-wide-Patient-Flow.aspx
[2] Mayo Clinic COVID-19 Predictive Analytics Task Force, Pollock BD, Carter RE, et al. Deployment of an Interdisciplinary Predictive Analytics Task Force to Inform Hospital Operational Decision-Making During the COVID-19 Pandemic. Mayo Clin Proc. 2021;96(3):690-698. https://www.mayoclinicproceedings.org/article/S0025-6196(20)31482-8/fulltext
[3] Weissman GE, Crane-Droesch A, Chivers C, et al. Locally Informed Simulation to Predict Hospital Capacity Needs During the COVID-19 Pandemic. Annals of Internal Medicine. Volume 173, Issue 1: 21-28. https://www.ncbi.nlm.nih.gov/pubmed/32259197
[4] Foley M, Kifaieh N, Mallon W. Financial Impact of Emergency Department Crowding. Western Journal of Emergency Medicine, Volume XII, no. 2: May 2011, 192-197. https://pubmed.ncbi.nlm.nih.gov/30193738/
[5] Reducing hospital readmissions with integrated COPD care. Philips case study. [Results are specific to the institution where they were obtained and may not reflect the results achievable at other institutions.] https://www.philips.com/a-w/about/news/archive/case-studies/20191001-reducing-hospital-readmissions-with-integrated-copd-care.html

Share on social media
Topics
Author

Henk van Houten
Former Chief Technology Officer at Royal Philips from 2016 to 2022